Abstract

Background:
The addition of sorafenib to standard induction and consolidation therapy in newly diagnosed patients (pts) ≤60 years (yrs) with acute myeloid leukemia (AML) led to significant prolongation of event-free survival (EFS) and relapse-free survival (RFS) in the randomized placebo-controlled SORAML trial (NCT00893373). After a median follow-up of 3 yrs, a benefit for sorafenib treated pts was observed also in overall survival (OS), but this difference was not significant. Here, we present updated survival data and information on relapse treatment and outcome.
Methods:
In the SORAML trial, 267 newly diagnosed untreated fit AML pts up to 60 yrs of age and irrespective of FLT3 mutation status received two cycles of induction chemotherapy with DA (daunorubicin 60 mg/m2 days 3-5 plus cytarabine 100 mg/m2 cont. inf. days 1-7), followed by three cycles of high-dose cytarabine consolidation (3 g/m2 b.i.d. days 1, 3, 5). Allogeneic stem cell transplantation (SCT) was scheduled for all intermediate-risk pts in first complete remission (CR) with a sibling donor and for all high-risk pts with a matched related or unrelated donor. At study inclusion, pts were randomized to receive either sorafenib (2x400 mg/day) or placebo as add-on to standard treatment in a double blinded fashion. Study medication was given on days 10-19 of DA I+II, from day 8 of each consolidation until 3 days before the start of the next consolidation and as maintenance for 12 months (mos) after the end of consolidation. The primary endpoint of the trial was EFS. The results after follow-up of 3 yrs were presented at ASH 2014 (Röllig et al., Blood 2014; 124: 6) and fully published (Röllig et al., Lancet Oncol 2015; 16: 1691-9). Here, we present the results after prolonged follow-up. For this analysis, information on remission and survival status, mode and outcome of relapse treatment including SCT were collected for all randomized pts and analyzed by standard statistical methods.
Results:
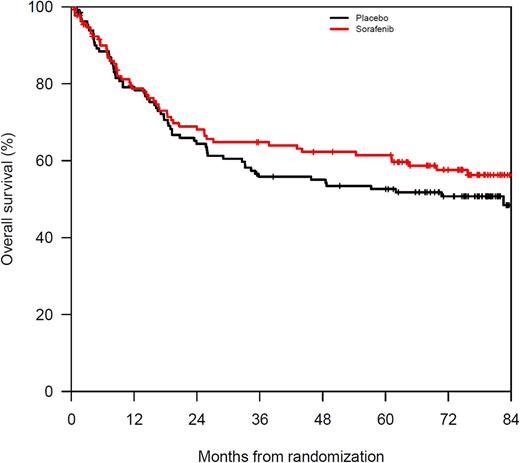
Of 267 treated pts, 134 were randomized in the sorafenib arm and 133 in the placebo arm with a resulting CR rate of 60% and 59%, respectively. After a median observation time of 78 mos, the primary study endpoint EFS in the placebo vs sorafenib arm was 9 mos vs 26 mos (HR 0.68, p=0.01) in univariate Kaplan Meier analysis. The beneficial effect of sorafenib on EFS was confirmed in multivariate Cox regression analysis with a HR of 0.61 (p=0.005). Median RFS in the placebo vs sorafenib arms was 22 vs 63 mos, corresponding to a HR of 0.64 (p=0.033). Exploratory analyses were performed in the 70 relapsing pts (40 after placebo vs 30 after sorafenib treatment). Among relapsing pts, 82% vs 73% achieved a second CR. In these two groups, 88% and 87% of pts received a SCT as part of salvage treatment. A lower proportion of pts in the placebo arm received a second SCT as salvage treatment (5% vs 13%). In the context of salvage SCT, the proportion of haploident donors in the placebo and sorafenib group was 3% vs 15% and the incidence of Grade 3/4 GVDH was 17% vs 0%. SCT-related non-relapse mortality (NRM) was similar in both groups, but the cumulative incidence of second relapse (CIR) was higher in the sorafenib group (35% vs 54% after 48 mos). Therefore, median OS from relapse in the placebo vs sorafenib groups were 27 mos vs 10 mos, corresponding to a HR of 1.68 (p=0.098). The projected median OS from randomization is 83 mos in the placebo arm and was not reached for the sorafenib arm, corresponding to a 5-year OS of 52% vs 61% (HR 0.81, p=0.263).
Conclusion:
Mature follow-up data confirms the antileukemic efficacy of sorafenib in younger AML pts with and without FLT3 mutation. The addition of sorafenib to standard chemotherapy resulted in a significantly longer EFS and clinically relevant 36% risk reduction for relapse or death. Five pts need to be treated (NNT) to prevent one relapse or death at 3 years and six pts at 5 yrs. Exploratory analyses in relapsing pts show that survival after relapse is shorter after sorafenib which might be due to i) a higher rate of second SCTs and a higher incidence of haploidentical SCT despite the lower frequency of severe GVHD, most likely by chance and not explainable by systematic reasons and ii) a lower response to salvage treatment after sorafenib therapy. Despite these observations, primary sorafenib treatment led to an OS benefit with a 19% risk reduction for death which was not statistically significant since this phase II trial was not adequately powered to detect OS differences.
Rollig: Bayer: Research Funding; Janssen: Research Funding. Hüttmann: Gilead, Amgen: Other: Travel cost; Bristol-Myers Squibb, Takeda, Celgene, Roche: Honoraria. Giagounidis: Acceleron: Consultancy; Celgene: Consultancy. Mackensen: AMGEN: Research Funding. Hänel: Roche: Honoraria; Novartis: Honoraria. Thiede: Roche: Consultancy; Novartis: Consultancy, Speakers Bureau; Bayer: Consultancy, Speakers Bureau; Agendix: Employment. Schetelig: Sanofi Aventis: Consultancy, Research Funding; Roche: Honoraria; Abbvie: Honoraria; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal